UCLA researchers used fluorescent colored proteins to trace how cardiomyocytes — cells in heart muscle that enable it to pump blood — are produced in mouse embryos. The findings could eventually lead to methods for regenerating heart tissue in human adults.
The research was published in the journal Nature Communications.
“Our ultimate goal is to be able to regenerate cardiomyocytes after an injury like a heart attack,” said Dr. Reza Ardehali, an associate professor of medicine in UCLA’s division of cardiology and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA. “But we’re first trying to learn from the embryonic heart.”
Cardiomyocytes make up most of the heart. During a heart attack, parts of the heart tissue are cut off from oxygen and nutrients. Cells in those regions of the heart die and are slowly replaced by scar tissue, which reduces the heart’s capacity to function.
While it has been known that cardiomyocytes are formed during embryonic development, scientists have been unsure until now whether new cardiomyoctyes are only created when existing cardiomyocytes divide, or whether cardiac progenitor cells — a type of stem cell — create new cardiomyocytes.
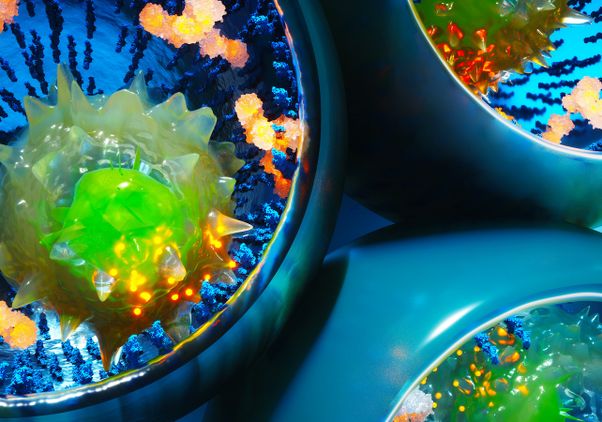
Ardehali and his colleagues, including Ngoc Nguyen, a UCLA graduate student and the study’s co-first author, used four different fluorescent-colored proteins to determine the origin of cardiomyocytes. When the cells divide, the resulting “daughter” cells maintain the same color as the parent cell.
“The system lets us see, over time, which cell populations give rise to new cells,” Nguyen said. “Compared to previous labeling methods that use only one or two different colors, this method allows us distinguish the role of different cells much more clearly.”
The team labeled different types of starting cells — including cardiomyocytes and cardiac progenitor cells — in mouse embryos by engineering the cells to contain genes for the fluorescent proteins. They turned the fluorescent labels on at different times during embryonic development and then watched how the colors spread through the developing heart as the embryos grew.
The scientists found that during early in utero development, most new cardiomyocytes come from cardiac progenitor cells rather than from existing cardiomyocytes. As a mouse fetus develops, however, the cardiac progenitor cells lose their ability, over the course of a few days or a week, to generate new cardiomyocytes.
“Previously, researchers hypothesized that you have these progenitor cells until a set point in development, and then they turn into mature cardiomyocytes,” Ardehali said. “We’ve shown that this process does not occur abruptly, but it is rather a gradual transition.”
The researchers also used the fluorescent proteins to study whether new heart cells arise after a heart injury. To do that, they simulated a heart attack in mice by surgically closing one of the heart arteries. They found that in newborn mice, the heart maintained a limited ability to regenerate cardiomyocytes after the artery was closed — even though its progenitor cells had matured. But when the heart attack was simulated in adult mice, the animals lacked that regenerative capability and couldn’t recover.
“If we can determine how these cardiomyocytes proliferate, we hope to harness that regenerative potential for the treatment of heart disease in humans,” Nguyen said.
The researchers have identified a handful of genes in the cardiomyocytes of newborn mice whose levels are different from those of adult mice; they are planning to study whether any of those genes are responsible for giving the cells the ability to regenerate.
The research was supported by grants from the California Institute for Regenerative Medicine; the National Institutes of Health; the American Heart Association; the Department of Defense; the Sarnoff Cardiovascular Research Foundation; and the Broad Stem Cell Research Center’s Research Award Program, Scholars in Translational Medicine Program and Rose Hills Foundation Training Program.