Researchers from UCLA's Jonsson Comprehensive Cancer Center have discovered that specific types of bacteria that live in the gut are major contributors to lymphoma, a cancer of the white blood cells.
Published online ahead of press today in the journal Cancer Research, the study was led by Robert Schiestl, member of the Jonsson Cancer Center and professor of pathology and laboratory medicine, environmental health sciences, and radiation oncology.
In rodents, intestinal bacteria influence obesity, intestinal inflammation and certain types of epithelial cancers. (Epithelial cancers affect the coverings of the stomach, liver or colon.) However, little is known about the identity of the bacterial species that promote the growth of, or protect the body from, cancer — or about their effect on lymphoma.
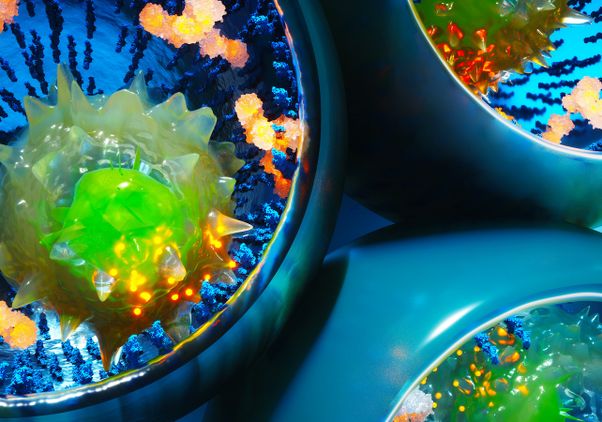
Up to 1,000 different species of bacteria (intestinal microbiota) live in the human gut. Intestinal microbiota number 100 trillion cells; over 90 percent of the cells in the body are bacteria. The composition of each person's microbiome — the body's bacterial make-up — is very different, due to the types of bacteria people ingest early in their lives, as well as the effects of diet and lifestyle.
Schiestl's group wanted to determine whether differences in peoples' microbiomes affect their risk for lymphoma, and whether changing the bacteria can reduce this risk. They studied mice with ataxia-telangiectasia (A-T), a genetic disease that in humans and mice is associated with a high rate of B-cell lymphoma. They discovered that, of mice with A-T, those with certain microbial species lived much longer than those with other bacteria before developing lymphoma, and had less of the gene damage (genotoxicity) that causes lymphoma.
"This study is the first to show a relationship between intestinal microbiota and the onset of lymphoma," Schiestl said. "Given that intestinal microbiota is a potentially modifiable trait, these results hold considerable promise for intervention of B-cell lymphoma and other diseases."
The scientists also were able to create a detailed catalog of bacteria types with promoting or protective effects on genotoxicity and lymphoma, which could be used in the future to create combined therapies that kill the bacteria that promote cancer (as antibiotics do) and increase the presence of the bacteria that protect from cancer (as probiotics do).
The work was supported by the National Institutes of Health, Jonsson Cancer Center, the Crohn's and Colitis Foundation of America, the Eli & Edythe Broad Center of Regenerative Medicine & Stem Cell Research, the Austrian Federal Ministry of Science and Research, NASA, University of California Toxic Substances Research and Teaching Program, and the UCLA Graduate Division.
UCLA's Jonsson Comprehensive Cancer Center has more than 240 researchers and clinicians engaged in disease research, prevention, detection, control, treatment and education. One of the nation's largest comprehensive cancer centers, the Jonsson center is dedicated to promoting research and translating basic science into leading-edge clinical studies. In July 2012, the Jonsson Cancer Center was once again named among the nation's top 10 cancer centers by U.S. News & World Report, a ranking it has held for 12 of the last 13 years.
For more news, visit the UCLA Newsroom and follow us on Twitter.